New findings also indicate that children who live in settings with a high burden of TB have a consistently high annual risk of developing TB infection throughout childhood.
An estimated 1.2 million children develop tuberculosis disease (TB) and 200,000 kids die from TB worldwide each year, but the risk of developing TB infection and disease throughout childhood remains under-studied. Furthermore, the majority of studies on the pediatric burden of TB are informed by data from patients in healthcare settings, rather than people in real-world, community settings.
A new study led by Boston University School of Public Health (BUSPH), the University of São Paulo, and the University of Cape Town sheds new light on this risk, with finding that there is a high risk of TB infection and disease in children up to 10 years old who live in areas where TB spread is common.
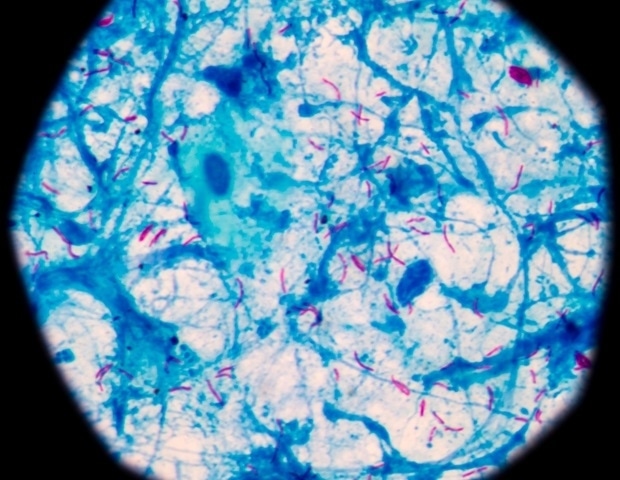
Published in The Lancet Child & Adolescent Health, the study is the first birth cohort study to assess TB infection and active TB disease during children’s first decade of life in high-burden settings. The new results found that there was a consistently high rate of annual TB infection among children in the study group-;between 4-9 percent-;and that more than 10 percent of children developed TB disease by the time they were 10 years old. The study builds upon a previous analysis by some of the researchers which also found high rates of TB infection and disease in children up to five years old.
These results are striking and show that children in these communities in South Africa are at extraordinarily high risk. Perhaps 1,000 to 2,000 South African children are at greater risk of TB than their young counterparts in the United States. It’s clearly an urgent health problem with both short and long-term impacts on these children and their families.”
Dr. Leonardo Martinez, study co-senior author, assistant professor of epidemiology at BUSPH
For the study, Dr. Martinez and colleagues observed and followed a birth cohort of 1,137 pregnant women and their 1,143 children enrolled in the Drakenstein Child Health Study and who were living near Cape Town, South Africa between 2012 and 2023. They tested the children for TB infection and disease at age 6 months, 12 months, and then annually for those who produce negative test results, as well as whenever they developed lower respiratory tract infection.
By eight years old, the team estimated that children’s cumulative risk of developing TB infection was a substantial 36 percent. New cases of TB disease were highest during the first year of life, and even though this risk decreased as children grew older, 1 in 10 children afflicted by TB disease by age 10 is still an alarming finding because it portends that this population will likely have weakened immune systems that may make them susceptible to future health issues and challenges later, both in young adulthood and in older age.
With TB drugs, TB disease is highly treatable, and the researchers found that preventative treatments were broadly effective for infected children who accessed this care-;but only a small proportion of the cohort did so. Most eligible children with TB infection did not receive preventive treatment, and the majority of those who developed TB disease had not received preventive medicine.
“Despite reasonable nutrition and almost no children living with HIV, there was an extraordinarily high, concerning rate of TB infection and disease in this cohort,” says co-senior author Dr. Heather Zar, principal investigator of the Drakenstein Child Health Study. Many children with TB disease were diagnosed when they presented with acute pneumonia, suggesting that in areas of high TB prevalence, children with pneumonia should be investigated for TB.”
As part of its Sustainable Development Goals, the World Health Organization has pledged by 2030 to reduce TB incidence by 80 percent and TB deaths by 90 percent, and to ease the financial burden among individuals and families dealing with this illness. Decreasing pediatric TB is a critical component of this goal, and one that requires a layered approach, the researchers say.
Much work still needs to be done to tackle the pediatric tuberculosis epidemic in South Africa and other high-burden countries, Dr. Martinez says. “If we are to reduce pediatric tuberculosis globally, a multisectoral approach is needed that brings together researchers, policymakers, healthcare workers, funders, and advocates to find comprehensive solutions.”
The study’s lead author is Dr. Fernanda Bruzadelli Paulino da Costa of the University of São Paulo. Coauthors include Dr. Mark P. Nicol, Maresa Botha, and Lesley Workman of the University of Western Australia, and Ricardo Alexandre Arcêncio of the University of São Paulo.
Source:
Journal reference:
da Costa, F. B. P ., et al. (2024) Mycobacterium tuberculosis infection and tuberculosis disease in the first decade of life: a South African birth cohort study. The Lancet Child & Adolescent Health. doi.org/10.1016/S2352-4642(24)00256-6.
Source link : News-Medica