Researchers observed the most significant gut microbiome instability in individuals who developed arthritis within 10 months of diagnosis, while those diagnosed 10-15 months later had a more stable profile.
In a recent study published in the journal Annals of the Rheumatic Diseases, researchers from the United Kingdom explored gut microbiome changes in individuals at high risk for rheumatoid arthritis. By comparing gut bacteria profiles between individuals who eventually developed rheumatoid arthritis and those who did not, the researchers aimed to identify the microbial indicators that could signal early disease development.
Background
Rheumatoid arthritis is a chronic autoimmune disease that affects mainly the joints and sometimes other organs. Though its exact cause remains unclear, the onset of rheumatoid arthritis is believed to involve immune responses triggered by environmental and genetic factors. Studies have found that antibodies targeting proteins modified in specific ways often appear before symptoms, hinting at early immune activation preceding the disease.
Furthermore, smoking and gum disease are associated with rheumatoid arthritis, further suggesting that localized inflammation at mucosal sites, like the lungs or mouth, might initiate disease-related immune responses. Evidence from various studies also points to the gut microbiome’s potential role in the development of rheumatoid arthritis. While certain bacterial groups, such as Prevotella species, have been linked to rheumatoid arthritis, the findings from various studies about these microbial associations have been conflicting.
About the study
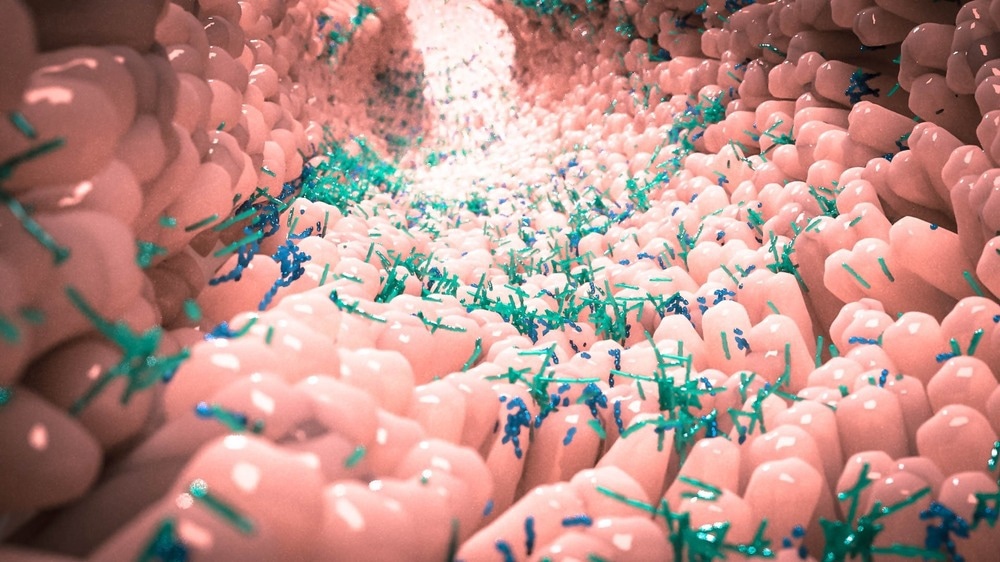
The present study examined gut microbial changes in people at risk for rheumatoid arthritis, focusing on the diversity and stability of gut bacteria over time to identify consistent microbial signatures associated with disease progression. The researchers used a combination of cross-sectional and longitudinal designs to analyze gut microbiome changes in individuals at risk for rheumatoid arthritis.
The participants included individuals with anti-cyclic citrullinated peptide (CCP) antibodies, which is a marker of rheumatoid arthritis risk. The study also included participants who had musculoskeletal pain without clinical arthritis, patients who were recently diagnosed with rheumatoid arthritis, and healthy controls. The researchers recruited individuals with diverse backgrounds and factors such as diet, lifestyle, and bowel habits.
Each participant provided stool samples, and data on demographic factors, antibody levels, and lifestyle factors were collected. The stool samples were analyzed for bacterial diversity and composition using two deoxyribonucleic acid (DNA) sequencing approaches. The 16S ribosomal ribonucleic acid (rRNA) amplicon sequencing targeted specific bacterial genes for broad taxonomic classification, while shotgun metagenomic sequencing was performed to obtain more detailed insights into bacterial strains and functional genes.
The researchers also performed diversity analysis to compare bacterial richness among participant groups, focusing on alpha diversity, which assesses the species diversity within samples, and beta diversity, which compares species diversities between samples. Various statistical analyses were then used to identify the bacterial taxa associated with the progression of rheumatoid arthritis.
Mixed-effects linear models were applied to capture changes in gut bacteria across time points for each participant while adjusting for demographic variables and antibody levels. Additionally, comparisons were also conducted to assess microbial stability over time, particularly within 10 months of the onset of rheumatoid arthritis. Furthermore, variability within the gut microbiome was analyzed to track shifts in bacterial composition before disease onset, identifying potential microbial markers linked to the development of rheumatoid arthritis.
Results
The study found that gut microbiome profiles differed significantly between individuals who eventually developed rheumatoid arthritis and those who did not. At baseline, the anti-CCP-positive individuals at risk for rheumatoid arthritis had lower gut microbiome diversity compared to healthy controls.
Furthermore, those who eventually developed rheumatoid arthritis showed greater changes in microbial diversity, and their gut microbiome was observed to become less stable within 10 months before the clinical symptoms of rheumatoid arthritis appeared.
The study revealed that specific strains within the Prevotellaceae family were more abundant in the individuals who eventually developed rheumatoid arthritis, while the other strains were less common, suggesting that Prevotella species played a complex role in rheumatoid arthritis. Individuals who eventually developed rheumatoid arthritis exhibited an accumulation of certain gut bacteria, including those from the Prevotellaceae family, within months of developing symptoms.
Furthermore, the findings highlighted an increase in the pathways related to amino acid and energy metabolism among the individuals who developed rheumatoid arthritis, indicating that metabolic shifts accompanied the microbiome changes associated with rheumatoid arthritis.
Moreover, the longitudinal analyses showed that the gut microbial diversity decreased progressively as individuals approached the onset of rheumatoid arthritis. The researchers conducted a stability analysis, which found that the microbiome became increasingly unstable and disordered in those close to developing rheumatoid arthritis, suggesting that these microbial shifts could be the early clinical signs of rheumatoid arthritis.
Conclusions
Overall, the results suggested that specific changes in gut microbiome composition and diversity, especially among anti-CCP-positive individuals, could be early indicators of increased risk of rheumatoid arthritis.
The observed microbial shifts could be considered potential markers for early rheumatoid arthritis. These findings also support the need for further exploration of gut bacteria as a tool for predicting and preventing rheumatoid arthritis.
Journal reference:
Source link : News-Medica