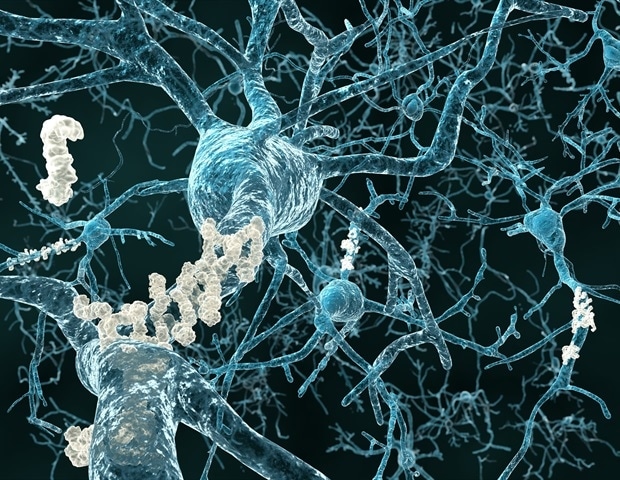
A Penn Medicine-led consortium of radiology and chemistry researchers across the United States will advance imaging of diseases like Parkinson’s by testing radiotracers they identified that illuminate α-synuclein (αSyn) or 4R tau proteins on positron emission tomography (PET) scans. Armed with a five-year, $30 million grant from the National Institutes of Neurological Disease and Stroke, researchers hope that improved imaging will expand the number of neurological disorders that can be diagnosed with PET scans, track their progression over time, and more accurately measure a patient’s response to treatments.
PET imaging uses a radioactive drug (tracer) that binds to certain proteins or sugars, to show areas of the body that have higher levels of chemical activity, indicating disease. It was just over a decade ago that researchers first identified a radiotracer that could be used to detect the presence of amyloid protein plaques in the brain, which are among the markers for Alzheimer’s disease. As new amyloid-clearing Alzheimer’s drugs have come to market, such as lecanemab, this radiotracer has become integral for diagnosing Alzheimer’s disease and tracking the progress of the drug.
Now, Robert Mach, PhD, the Britton Chance Professor of Radiology, will lead a collaboration with experts around the country to pursue similar tracers for Parkinson’s and several other diseases that are characterized as “proteinopathies,” which occur when certain proteins “misfold,” and aggregate on the brain. Called the Center Without Walls, the project connects radiology, chemistry, and neurology experts from The University of California-San Francisco, the University of Pittsburgh, Washington University-St. Louis, and Yale University to develop two different radiotracers: one that will bind to a protein in the brain known as αSyn for the imaging of Parkinson’s and multiple system atrophy, and the other that will bind to the protein 4R tau for imaging frontotemporal degeneration and progressive supranuclear palsy.
“Due to the sheer number of possible molecules that could be used, the process of developing new radiotracers has been slow and complicated, like finding a needle in a haystack,” said Mach. “The Center Without Walls combines clinical, scientific, imaging, and computational expertise from across institutions to develop a creative solution for this problem and has already resulted in clinical trials for three radiotracers that we identified. We hope that this collaborative model can help develop radiotracers that fundamentally change how we diagnose and treat diseases like Parkinson’s.”
In the first five years of the collaboration, investigators from the University of Pennsylvania department of Chemistry, led by E. James Petersson, PhD, a professor of Chemistry, Biochemistry, and Biophysics, developed a state-of-the-art computational chemistry tool that evaluates the millions of potential molecules and identifies a few hundred to test. The tool then models how these molecules bind to and interact with the proteins, and identify which ones are most likely to be most effective.
Using this method, the hundreds of potential molecules were narrowed down to just three: two for αSyn and one for 4R tau. During the next five years of the project, investigators will begin clinical trials of the three tracers in human subjects.
“Now that we’ve shown this computational chemistry model can identify the right molecules to bind to and trace αSyn, our hope is that soon we can plug any protein target into the model and rapidly develop an effective radiotracer, and get these tracers into clinic sooner, so that we can better diagnose and manage a range of complicated diseases.”
This research is funded by the National Institutes of Neurological Disorders and Stroke (U19NS110456).
Source link : News-Medica