Scientists at City of Hope®, one of the largest and most advanced cancer research and treatment organizations in the U.S. with its National Medical Center named top 5 in the nation for cancer by U.S. News & World Report, have collared a tricky culprit that helps cancer cells evade CAR T cell therapy.
CAR T cell therapy harnesses the immune system to seek out and kill tumor cells. This treatment is used in certain types of leukemia and lymphoma -; blood cancers. Some wily cancer cells, however, have learned how to hide from the immune system to avoid destruction. The study published today in the journal Cell could lead to more personalized therapies that improve cancer patients’ survival.
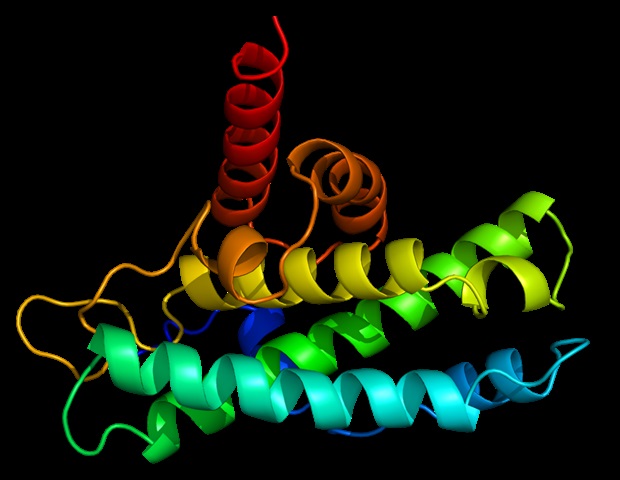
The researchers identified a protein called YTHDF2 that plays a starring role in advancing the development of blood cancers. City of Hope then created a new medicinal compound called CCI-38, which targets and suppresses YTHDF2, reducing the growth of aggressive blood cancers. The approach improves the likelihood of successful cancer treatment.
We believe that using CCI-38 to target YTHDF2 will significantly enhance the effectiveness of CAR T cell therapy on blood cancer cells.”
Jianjun Chen, Ph.D., Simms/Mann Family Foundation Chair in Systems Biology and the director of the Center for RNA Biology and Therapeutics at Beckman Research Institute of City of Hope
“One of the challenges in treating blood cancers is a phenomenon called ‘antigen escape.’ A key target for these therapies is a protein called CD19 found on the cancer cells,” added Dr. Chen, corresponding author of the new study.
However, in 28-68% of cases, the cancer cells lower or lose this CD19 marker, making treatments less effective. Although researchers are working on strategies to target multiple components, nearly half of patients are still affected by this issue.
YTHDF2 switches on genes that help cancer cells produce a stable energy source to fuel the cells’ ability to grow and spread. Moreover, this protein helps cancer cells conceal themselves by reducing the presence of antigen biomarkers that normally trigger the immune system to detect and attack cancer. Lastly, excess YTHDF2 works like a werewolf’s bite to transform blood cells from healthy to cancerous in mouse studies.
“Reducing the need for follow-up treatments could lead to better long-term survival and less relapse for our patients while lowering side effects and medical costs,” said Xiaolan Deng, Ph.D., an associate research professor in systems biology at Beckman Research Institute of City of Hope and a co-corresponding author of the study.
City of Hope, a recognized leader in CAR T cell therapies for glioblastoma and other cancers, has treated more than 1,600 patients since its CAR T program started in the late 1990s. The institution continues to have one of the most comprehensive CAR T cell clinical research programs in the world.
“Unraveling the biology underlying YTHDF2’s function will help us develop new strategies to prevent tumor cells from escaping immune surveillance,” said Zhen-Hua Chen, Ph.D., a staff scientist in systems biology at Beckman Research Institute of City of Hope and first author of the study. “This could lead to personalized approaches for patients whose blood cancers don’t respond to initial treatment or who relapse after initial response to T cell-based immunotherapy.”
The City of Hope team has filed a patent application covering critical aspects of this work, which holds implications for improving care for patients with other cancers and severe autoimmune diseases. The next phase of research will focus on improving CCI-38’s safety and effectiveness, exploring new methods to drive YTHDF2 out of cancer cells, and developing clinical trials.
Source:
Journal reference:
Chen, Z., et al. (2024) YTHDF2 promotes ATP synthesis and immune evasion in B cell malignancies. Cell. doi.org/10.1016/j.cell.2024.11.007.
Source link : News-Medica