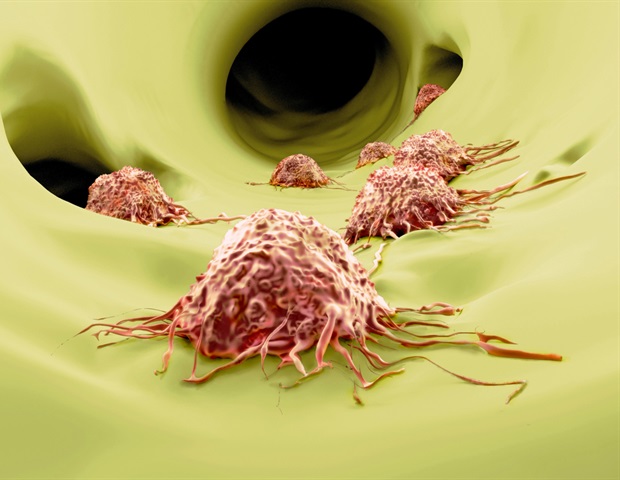
Understanding in depth how tumors evolve to become malignant is the objective of the latest study led by the Cell Plasticity in Development and Disease laboratory, directed by ángela Nieto at the Institute for Neurosciences (IN), a joint center of the Spanish National Research Council (CSIC) and the Miguel Hernández University (UMH) of Elche. This work, recently published in the journal Nature Cancer, demonstrates that within each tumor, groups of cells receive instructions to spread malignantly throughout the body. Other groups of cells are responsible for combating the damage caused by the cancerous tumor.
The laboratory led by ángela Nieto at the IN in Alicante (Spain) has studied for 20 years a process called epithelial-mesenchymal transition (EMT), which, during embryonic development, allows the migration of cells to different destinations to form organs and tissues. This same program is used by cancer to spread its cells and give rise to metastases and tumors in other organs that cause more than 90% of the deaths associated with this disease.
Nieto’s team’s deep knowledge of this process also led them to discover that, in adults, this program is a defense mechanism that cells use to protect themselves when they detect damaged tissue and repair it. However, when the damage is chronic, the cells can no longer repair; they secrete collagen that accumulates and develops fibrosis that degenerates the organ.
Now, in this work, IN researchers have shown that in cancer, both the embryonic development and adult programs are activated unexpectedly:
The two programs are activated in the tumor, but in different populations. That is, we observe opposing pro and antitumor programs that are working at the same time.”
ángela Nieto at the IN in Alicante (Spain)
Along these lines, researcher Khalil Kass Youssef, the first author of the article, highlights that the same cell can respond in one way or another: “When the epithelial-mesenchymal transition is activated with the two programs in different cells, intratumoral heterogeneity occurs. Ours is the first confirmation of this phenomenon.” Furthermore, researchers have observed that the two cell populations have very different locations within the tumor. The cells that activate the embryonic-like EMT process are found in the periphery of the tumor, while the cells that activate the repair process are concentrated in the center of the tumor.
A critical factor in cellular dedifferentiation
When cells differentiate during the development of an individual, they receive a series of cellular identity instructions, which determine the functions they will carry out throughout their life. The results of this work show that EMT is a mechanism of cellular plasticity that allows adult cells to dedifferentiate so that they can act in another way: “If the cell is highly differentiated, it cannot do anything more than what it already knows. So, when it must respond to a stimulus such as, for example, damage, it has to reverse those instructions a little to be able to perform other functions”, explains Nieto and highlights that this plasticity mechanism is essential to carry out regenerative processes.
The results of this work suggest that the transcription factor Snail1 plays a vital role in this process since it appears first and in both EMT trajectories. On the other hand, researchers have proven that the transcription factor Prrx1 is decisive for the dissemination trajectory since when they eliminate this gene, the tumor’s metastatic capacity disappears.
The experts observed that blocking the dissemination of EMT trajectory reduces metastasis and leads to more cells being incorporated into the inflammatory EMT trajectory, which favors the recruitment of a type of macrophages responsible for fighting cancer cells. Researcher Khalil Kass Youssef emphasizes the significance of these results: “We have confirmed that both EMT trajectories are interdependent. This is a significant finding that opens opportunities for the design of new therapeutic strategies to treat aggressive types of cancer that are highly metastatic and very resistant to current therapies”.
Scientists have carried out this study using three mouse models: an embryonic model to study the development of the neural crest in embryos, an adult model of renal fibrosis, and, finally, a model of breast cancer. Through single-cell analysis techniques and computational data analysis, for which Nitin Narwade, computational scientist in the group led by Nieto, has collaborated with researcher José López-Atalaya, who directs the Cellular Plasticity and Neuropathology laboratory at the IN, the experts were able to define all the pro and antitumor cell states. Using machine learning, experts made predictions to determine the evolution of cancer cells, which they then validated with experimental studies in animal models.
Furthermore, with Aida Arcas, also from Nieto’s laboratory, and Professor Gema Moreno Bueno from the Sols-Morreale Biomedical Research Institute (IIBM-CSIC-UAM) and the MD Anderson Foundation (both in Madrid), the data from the animal models have been able to be correlated with patient data. ‘We have confirmed that all the cellular states of the two trajectories discovered in the animal models can be identified in human tumors, particularly in triple-negative breast cancer, which has the worst prognosis”, explains Moreno Bueno.
This work has been possible thanks to funding from the Spanish Ministry of Science, Innovation and Universities, the Scientific Foundation of the Spanish Association Against Cancer (AECC), the Carlos III Health Institute, the PROMETEO Programme of the Generalitat Valenciana, the European Research Council (ERC), the Spanish State Research Agency through the “Severo Ochoa Program” for Centers of Excellence in R&D, the European Molecular Biology Organization (EMBO), and the Horizon 2020 Research and Innovation Programme of the European Union NEUcrest within the framework of the Marie Skłodowska-Curie actions.
Source:
Journal reference:
Youssef, K. K., et al. (2024). Two distinct epithelial-to-mesenchymal transition programs control invasion and inflammation in segregated tumor cell populations. Nature Cancer. doi.org/10.1038/s43018-024-00839-5.
Source link : News-Medica