Artificial intelligence is transforming breast cancer screening by uncovering novel mammographic features linked to risk, paving the way for more precise prevention and risk-reducing strategies.
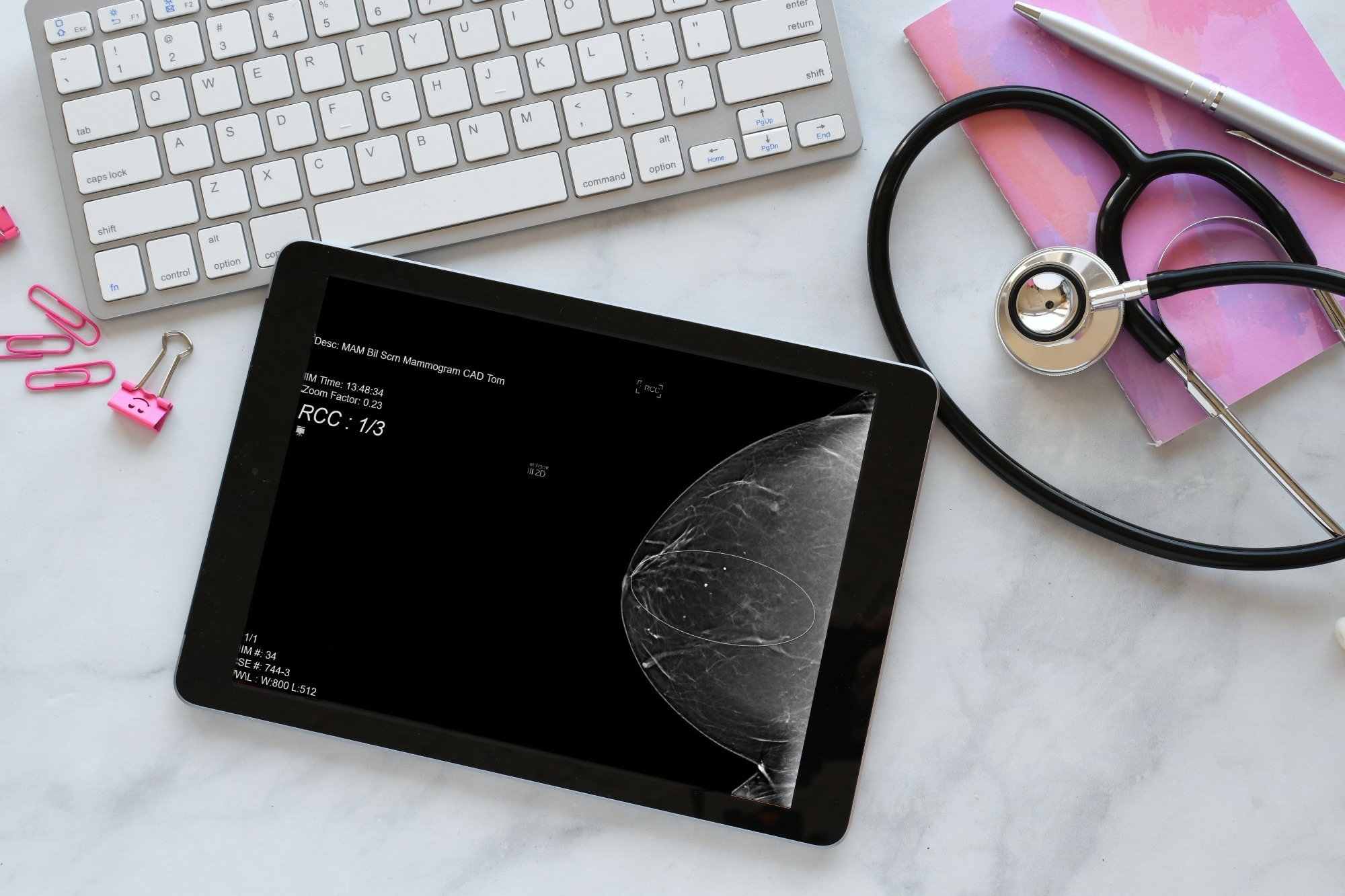
Study: Artificial intelligence improves mammography-based breast cancer risk prediction. Image Credit: MargJohnsonVA/Shutterstock.com
In a recent study published in Trends in Cancer, researchers summarized how artificial intelligence (AI) improves mammography-based prediction of breast cancer risk.
Introduction
The possibility of predicting future diagnosis of breast cancer using mammograms has intrigued many clinicians and scientists since the publication of a landmark study in 1976.
Accordingly, breast cancer risk could be determined solely based on the parenchymal pattern observed on mammography. These patterns, now referred to as mammographic or breast density, relate to the appearance of dark and light areas on a mammogram.
Breast tissue appearing dark (on a mammogram) is considered radiologically non-dense, while white is considered dense. The dense areas mainly comprise stroma and epithelium, collectively known as fibroglandular tissues, whereas non-dense areas predominantly comprise adipose tissue.
Individuals with an increased mammographic density for their body mass index and age have an increased breast cancer risk.
Moreover, such individuals have an additional complication, i.e., the masking effect, wherein greater mammographic density makes breast cancer detection harder.
In a significant refinement to mammography-based risk prediction, AI methods can uncover mammographic features, which are specific parenchymal patterns and stronger risk predictors. In the present study, researchers discussed advances in AI-based breast cancer risk prediction.
AI-generated mammographic features
Studies assessing relationships between AI-generated mammographic features and breast cancer risk are observational, and the measured associations do not necessarily imply causality. Notably, AI tools pinpoint areas with a high-risk score on mammograms.
However, since these areas do not appear suspicious in conventional radiology readings, it could be difficult to describe them as radiological findings.
As such, AI-generated features remain a “black box,” and their reproducibility beyond the training and testing sample sets is challenging. Besides, it is critical to uncover the pathobiology associated with mammographic features and the mechanisms linking them to breast cancer.
This will also be paramount to establishing their relevance to breast cancer risk and efforts to mitigate the risk.
A recent trial detected 36 breast cancers in 559 magnetic resonance imaging (MRI)-based screens of females with a negative screening mammogram and increased AI-based risk scores. These findings indicate that some mammographic features are suggestive of early malignancy.
Nevertheless, the identity of mammographic features remains unclear. Therefore, research must focus on developing novel approaches to uncover and characterize the pathobiology of mammographic features.
Implications for screening and risk mitigation strategies
Mammographic density has attracted significant interest due to its inclusion in risk prediction algorithms, masking effect, and potential use as a biomarker. This interest will intensify now with the advent of mammographic features.
Moreover, this research provides opportunities to identify individuals at the highest risk of breast cancer and separate them from others at risk of having breast cancer missed due to the masking effect.
Individuals with high-risk mammographic features could benefit from more frequent screening and risk-reducing medicines. That is, longer intervals between screening could be provided to those with a low risk of breast cancer in the next five years.
In addition, an individual with increased mammographic density but without high-risk mammographic features could benefit from supplemental imaging.
Mammographic features also provide opportunities for risk-reducing strategies. For instance, anti-estrogens like tamoxifen decrease the risk of breast cancer and may operate by reducing mammographic density.
However, it is unknown whether anti-estrogens or other drugs could modify mammographic features. Further, any risk-reducing medicine will need evidence from randomized clinical trials that reduced risk occurs from its effect on mammographic features.
Conclusion
AI research has uncovered novel features that might explain a large proportion of short-term associations between breast cancer risk and mammographic density. However, this does not imply that mammographic density is no longer a risk factor.
Nevertheless, stronger risk factors can be detected on a mammogram that better pinpoint changes in parenchymal patterns preceding breast cancer detection.
Further research is needed to explore the causal links between mammographic features, mammographic density, and breast cancer risk and inform risk-reducing strategies.
Source link : News-Medica